Hypoglycemia, Explained
Hypoglycemia (also known as low blood sugar or low glucose) more commonly affects people living with type 1 diabetes, but can affect those with type 2 diabetes as well.
This article is designed to help you understand the signs, symptoms and treatments for hypoglycemia, or ‘low’ as it’s often referred to.
What is hypoglycemia?
Hypoglycemia is when the level of glucose in the bloodstream is too low.
The non-medical term for hypoglycemia is low blood sugar, or low blood glucose. Some people might simply refer to themselves as ‘low’.
In general, a blood glucose reading below 70 mg/dl is considered ‘low’.
These can usually be treated quickly, but if left untreated glucose levels can continue to fall and become dangerous.
The body, and in particular the brain, relies on glucose to function properly - if you’ve ever had a hypo, you’ll know that it doesn’t feel very nice!
Why do people with type 1 diabetes have hypoglycemia?
If you experience hypos regularly, you’re not alone - most people with type 1 diabetes have at least one or two episodes of mild hypoglycemia a week.1
As you’ll likely know if you live with type 1 diabetes or care for someone with type 1 diabetes, your pancreas no longer produces insulin, or produces very little.
But insulin is needed to take glucose from the bloodstream to elsewhere in the body, where it can be used for energy. So, a person with diabetes has to take insulin manually via an injection or insulin pump.
Causes of hypoglycemia
Predicting the exact insulin dose your body needs throughout the day and night isn’t easy, so sometimes there will be too much insulin in the bloodstream.
As well as taking too much insulin, mis-timed, skipping or delaying meals, exercise and alcohol are other common contributors to episodes of hypoglycemia.2
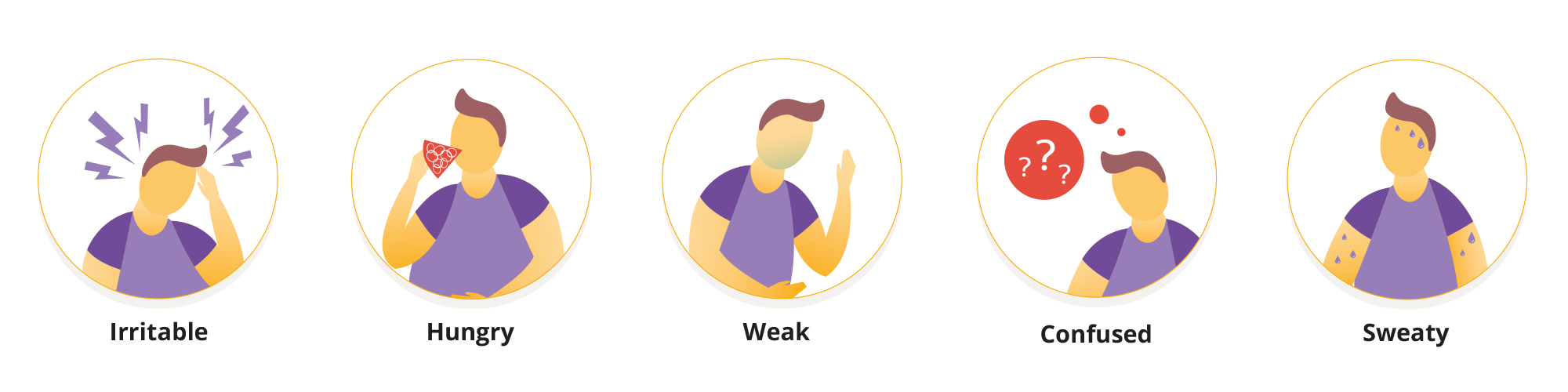
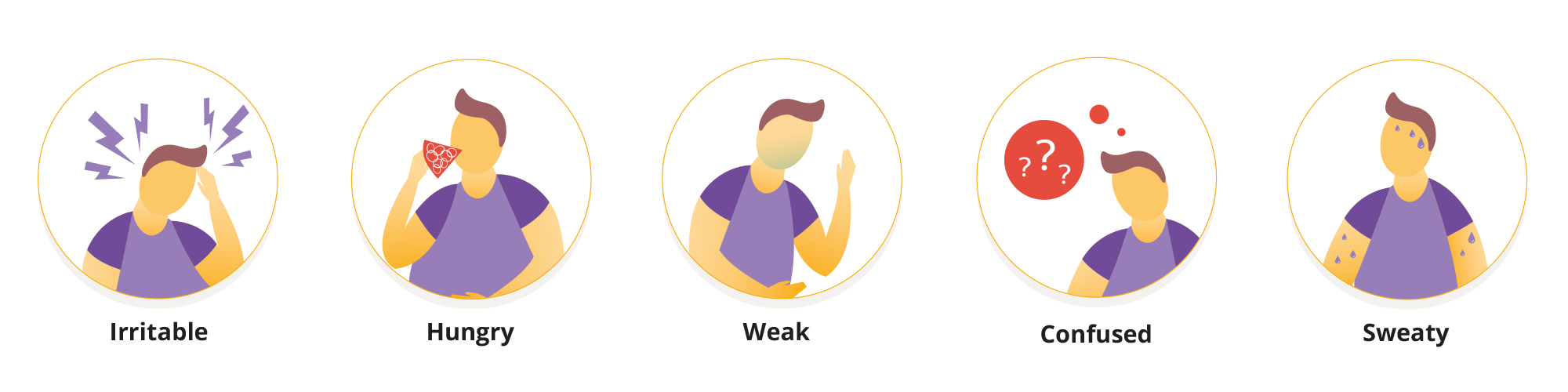
Symptoms of hypoglycemia2
Symptoms of low blood sugar can come on quickly and can vary from person to person.
Repeated episodes of low blood sugar can lead to hypoglycemia unawareness or even high blood glucose, if worry or fear of lows keeps you from taking your insulin and/or other diabetes medications. It’s worth talking to your healthcare provider if you’re concerned about or having repeated low glucose levels.
In general, symptoms might include: 2
- Shaking
- Dizziness
- Becoming easily irritated, tearful, anxious or moody
- Hunger
- Blurred vision
- Difficulty concentrating
- Weakness
- Confusion
- Sweatiness
- Changes in behavior
- Palpitations
As your blood glucose level drops lower, you are at increased risk of fainting (passing out).
Checking your glucose level frequently by taking a finger prick test, or by tracking it with a continuous glucose monitor (CGM) or glucose sensor can help you verify your symptoms and see if your glucose is actually low or heading low.
This is particularly important if you’re changing your medications, routine or crossing time zones.
We have more advice and information about traveling with diabetes here.
It’s important to carry some form of fast acting glucose with you. Glucose tablets, juice, and/or a glucagon kit are all good options.
Treating hypoglycemia for yourself3
If your blood glucose is low, follow these steps from the CDC: Treatment of Low Blood Sugar (Hypoglycemia)
Step 1: Carbohydrates
Eat or drink something that contains carbohydrates to bring your blood glucose back up into the normal level.
How much carbohydrate you need will depend on how low your blood glucose has dropped, and your age. In general, follow the 15-15 rule. But young children, especially infants and toddlers, may need less than 15 grams of carbs.
Step 2: Check your blood glucose
Check your blood glucose level after 10-15 minutes to see if it’s improved.
If it’s still low, eat a further 10-15 grams of carbohydrate and keep checking your glucose level every 15 minutes until it starts to rise and your glucose is within your target range.
Step 3: Balanced snack or meal
15 grams of carbohydrate equates to about 3-4 glucose tablets, or 4 oz (½ cup) of non-diet soda or fruit juice.
Once your blood sugar is back in the standard range, eating a balanced snack or meal with protein and carbs can help prevent another drop in blood sugar levels.
You can usually treat your own mild hypoglycemia, but you should speak to your healthcare provider team if you’re experiencing hypos frequently.
Severe hypoglycemia4
Severe hypoglycemia (in clinical terms) is when your glucose drops below 55 mg/dL. Sometimes your glucose is so low that it may require assistance of another person to actively administer carbohydrates, glucagon, or take other corrective actions.
If your blood glucose drops to a very low level, you may start to have problems walking, talking or seeing.
It’s a good idea to ask someone for help, especially if you’re unable to test your blood glucose, or you’re worried you might faint (pass out).
It’s helpful if your friends, family and colleagues know what to do if your blood glucose drops low, to help you feel safe in case you’re unable to treat the hypo by yourself.
Treating someone else’s low blood sugar
If someone is unable to respond to commands, cannot eat or drink sugar or falls unconscious, call 911 for an ambulance.
A glucagon injection is the best way to treat a severe low and is available by prescription. Speak with your doctor to always have a glucagon kit and make sure you know how to use it.
This may all sound very serious, but it’s good to be equipped with the right information in case a severe hypo happens - to you or to someone else.
How can Omnipod® help?
Omnipod is an insulin management system designed for people living with insulin requiring diabetes including type 1 and type 2 diabetes.
Omnipod provides continuous insulin delivery through a tubeless, waterproof* insulin pump called a Pod—all with no multiple daily injections. The Pod is a small device that you fill with insulin and wear directly on your body. Each Pod holds up to 3 days (72 hours) of insulin. The Pod receives insulin delivery instructions from the PDM or Controller. It then delivers insulin into your body through a small, flexible tube called a cannula.
The Omnipod® 5 Automated Insulin Delivery System offers all these benefits, but it also integrates with compatible CGMs or sensors. Each Pod is equipped with SmartAdjust™ technology, an algorithm that automatically increases, decreases, or pauses insulin every 5 minutes, based on your customized target—helping to protect against highs and lows, day and night.5-6
Continue reading:
Related Articles
References and Disclaimers
*The Pod has an IP28 rating for up to 25 feet for 60 minutes. The Personal Diabetes Manager and Controller are not waterproof.
1- Rory J. McCrimmon, Robert S. Sherwin; Hypoglycemia in Type 1 Diabetes. Diabetes 1 October 2010; 59 (10): 2333–2339. https://doi.org/10.2337/db10-0103
2- Low Blood Glucose (Hypoglycemia) - NIDDK: https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/low-blood-glucose-hypoglycemia]
3- Treatment of Low Blood Sugar (Hypoglycemia) | Diabetes | CDC: https://www.cdc.gov/diabetes/treatment/treatment-low-blood-sugar-hypoglycemia.html]
4- American Diabetes Association Professional Practice Committee; 6. Glycemic Goals and Hypoglycemia: Standards of Care in Diabetes—2025. Diabetes Care 1 January 2025; 48 (Supplement_1): S128–S145. https://doi.org/10.2337/dc25-S006
5- Brown et al. Diabetes Care (2021). Study in 240 people with T1D aged 6 - 70 years involving 2 weeks standard diabetes therapy followed by 3 months Omnipod 5 use in Automated Mode. Average overnight time (12AM-6AM) with high blood glucose in adults/adolescents and children for standard therapy vs Omnipod 5 = 32.1% vs. 20.7%; 42.2% vs. 20.7%. Average day time (6AM-12AM) with high blood glucose in adults/adolescents and children for standard therapy vs Omnipod 5 = 32.6% vs. 26.1%; 46.4% vs. 33.4%. Median overnight time (12AM-6AM) with low blood glucose in adults/adolescents and children for standard therapy vs Omnipod 5 = 2.07% vs. 0.82%; 0.78% vs. 0.78%. Median day time (6AM-12AM) with low blood glucose in adults/adolescents and children for standard therapy vs Omnipod 5 = 1.91% vs. 1.08%; 1.17% vs. 1.62%.
Sherr J, et al. Diabetes Care (2022). Study in 80 children with T1D aged 2 to 5.9 years involving 2 weeks standard diabetes therapy followed by 3 months Omnipod 5 use in Automated Mode. Average overnight time (12AM-6AM) with high blood glucose in children for standard therapy vs Omnipod 5 = 38.4% vs. 16.9%. Average day time (6AM-12AM) with high blood glucose in children for standard therapy vs Omnipod 5 = 39.7% vs. 33.7%. Average overnight time (12AM-6AM) with low blood glucose in children for standard therapy vs Omnipod 5 = 3.4% vs. 2.1%. Average day time (6AM-12AM) with low blood glucose in children for standard therapy vs Omnipod 5 = 3.4% vs. 2.6%.
6- Pasquel FJ, et al. Presented at: ADA; June 21-24, 2024; Orlando, FL. Prospective pivotal trial in 305 participants with T2D aged 18-75 yrs. Study included a 14-day standard therapy (ST) phase followed by a 13-week Omnipod 5 hybrid closed-loop phase. Mean time <70 mg/dL as measured by CGM: ST = 0.2%, 3-mo Omnipod 5 = 0.2%, P<001. Mean time >180 mg/dL as measured by CGM: ST = 54%, 3-mo Omnipod 5 = 34%, P<0.001. Comparison is relative change.
These modules are not a replacement for medical advice or training. Please always speak to a qualified healthcare professional about your options.
The information and other content provided in this article, or in any linked materials, are not intended and should not be construed as medical advice, nor is the information a substitute for professional medical expertise or treatment. If you or any other person has a medical question or concern, you should consult with your healthcare provider. Never disregard professional medical advice or delay in seeking it because of something that have read on this blog or in any linked materials. If you think you may have a medical emergency, call your doctor or emergency services immediately. The opinions and views expressed on this blog and website have no relation to those of any academic, hospital, health practice or other institution.



