All about hypoglycemia
Hypoglycemia (also known as hypoglycaemia or low blood sugar) commonly affects people living with type 1 diabetes.
This module is designed to help you understand the signs, symptoms and treatments for hypoglycemia, or ‘hypo’ as it’s often referred to.
What is hypoglycemia?
Hypoglycemia, hypoglycaemia or hypo, is when the level of glucose in the bloodstream is too low.
The non-medical term for hypoglycemia is low blood sugar, or low blood glucose. Some people might simply refer to themselves as ‘low’.
In general, a blood glucose reading below 4 mmol/l (70 mg/dl) is considered ‘low’.
Hypos can usually be treated quickly, but low blood glucose can also become dangerous if left untreated and glucose levels continue to fall.
The body, and in particular the brain, relies on glucose to function properly - if you’ve ever had a hypo, you’ll know that it doesn’t feel very nice!
Why do people with type 1 diabetes have hypoglycemia?
If you experience hypos regularly, you’re not alone - most people with type 1 diabetes have at least one or two episodes of mild hypoglycemia a week1.
As you’ll likely know if you live with type 1 diabetes or care for someone with type 1 diabetes, your pancreas no longer produces insulin, or produces very little.
But insulin is needed to take glucose from the bloodstream to elsewhere in the body, where it can be used for energy. So a person with diabetes has to take insulin manually via an injection or insulin pump.
Causes of hypoglycemia
Predicting the exact insulin dose your body needs throughout the day and night isn’t easy, so sometimes there will be too much insulin in the bloodstream.
As well as taking too much insulin, mis-timed, skipping or delaying meals, exercise and alcohol are other common contributors to episodes of hypoglycemia1,2.
Other factors including hot or humid weather, hormonal changes (like puberty or your menstrual cycle) and changes to routine or time zone also impact your blood sugar level1,2.
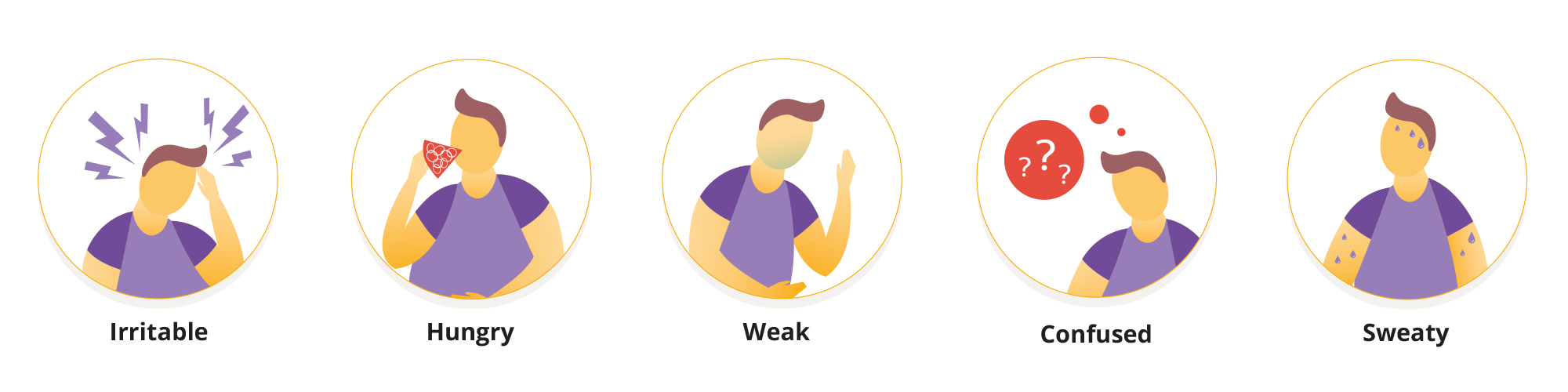
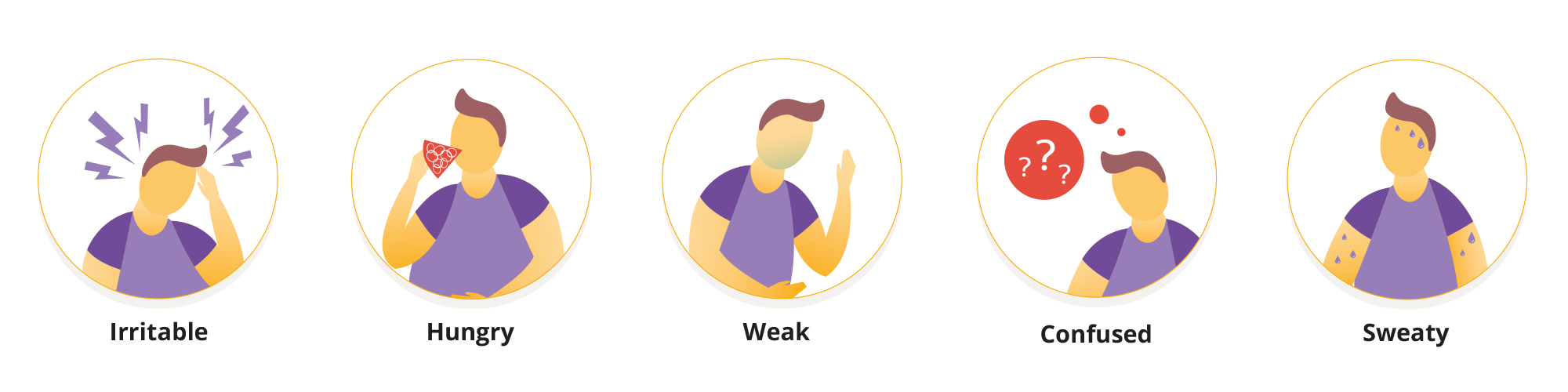
Symptoms of hypoglycemia
Everybody experiences hypos differently, and the speed at which your blood sugar level is dropping can also affect your symptoms.
Symptoms can change, the longer you live with type 1 diabetes - it’s worth talking to your diabetes healthcare team if you’re concerned about changing hypo awareness or hypo unawareness.
In general, symptoms might include2,3:
• Shaking
• Sweating
• Dizziness
• Hunger
• Blurred vision
• Difficulty concentrating
• Feeling anxious
• Changes in behaviour
• Tingling lips
• Turning pale
• Becoming easily irritated, tearful, anxious or moody
• Palpitations
As your blood glucose level drops lower, you are at increased risk of fainting (passing out).
The most important thing you can do to prevent this is to check your glucose level frequently by taking a finger prick test, or by tracking it with a continuous glucose monitor (CGM) or glucose sensor.
This is particularly important if you’re changing your routine or crossing time zones or climates.
We have more advice and information about travelling with diabetes here.
The other thing you can do to help you feel safe is to always carry some form of fast acting glucose with you. Glucose tablets, juice, and/or a glucagon kit are all good options.
Treating hypoglycemia for yourself
If your blood glucose is low, follow these steps from JDRF UK* to treat your hypo3: JDRF website
Eat or drink something that contains carbohydrates to bring your blood glucose back up into the normal level.
How much carbohydrate you need will depend on how low your blood glucose has dropped, and your age. In general, one carbohydrate portion (15 grams of carbohydrate) will bring your blood glucose level up by about 3 mmol/L (54mg/dL), but young children, especially infants and toddlers, usually need less than 15 grams of carbs.
Check your blood glucose level after 10-15 minutes to see if it’s improved.
If it’s still low, eat a further 10-15 grams of carbohydrate and keep checking your glucose level every 10 minutes until it starts to rise and you start to feel better
15 grams of carbohydrate equates to about three jelly babies, five glucose tablets, or 150ml of non-diet soft drink or fruit juice.
Once your blood sugar is back in the standard range, eating a healthy snack or meal can help prevent another drop in blood sugar levels.
You can usually treat your own mild hypoglycemia, but you might want to speak to your diabetes healthcare team if you’re experiencing hypos frequently.
Severe hypoglycemia
Severe hypoglycemia (in clinical terms) is an event requiring assistance of another person to actively administer carbohydrates, glucagon, or take other corrective actions.
If your blood glucose drops to a very low level, you may start to have problems walking, talking or seeing.
It’s a good idea to ask someone for help, especially if you’re unable to test your blood glucose, or you’re worried you might faint (pass out).
It’s helpful if your friends, family and colleagues know what to do if your blood glucose drops low, to help you feel safe in case you’re unable to treat the hypo by yourself.
Treating someone else’s low blood sugar
If someone is unable to respond to commands, cannot eat or drink sugar or falls unconscious, call 999 for an ambulance.
Put the person in the recovery position and do not put anything in their mouth, as they may choke3.
If a glucagon injection is available and you know how to use it, give it to them immediately2.
Glucagon is a hormone that triggers a release of stored glucose from your liver. People with type 1 diabetes can usually get this injection with a prescription from their doctor3.
They should wake up and start to feel better within 10-15 minutes of a glucagon injection. Give them a carbohydrate snack as soon as they’re able to take it.
This may all sound very serious, but it’s good to be equipped with the right information in case a severe hypo happens - to you or to someone else.
How can Omnipod® help?
Omnipod® is an insulin management system designed for people living with type 1 diabetes.
It’s what’s known as a patch pump, or Pod Therapy, which means being able to administer insulin without multiple daily injections and without the tubing associated with traditional insulin pumps.
Pod Therapy allows you to set temporary basal doses or even shut off insulin delivery completely, which can be helpful during an episode of hypoglycemia, and may even help reduce the frequency of hypos4.
The Omnipod® 5 Automated Insulin Delivery System offers all the same benefits, but it also integrates with compatible sensors to make automatic basal insulin adjustments.
Want to know more about Pod Therapy?
Right this way… Check the "What Is Pod Therapy?" module
Related Articles
References and Disclaimers
1 https://www.jdrf.org/t1d-resources/about/symptoms/blood-sugar/low/
2 https://www.nhs.uk/conditions/low-blood-sugar-hypoglycaemia/
3 https://jdrf.org.uk/information-support/managing-type-1-diabetes-3/hypos/
4 https://diabetesjournals.org/care/article/26/4/1079/23670/Insulin-Pump-TherapyA-meta-analysis
These modules are not a replacement for medical advice or training. Please always speak to a qualified healthcare professional about your options.



