Hyperglycemia, Explained
Hyperglycemia, or high blood glucose, can affect people living with diabetes. A person’s blood glucose will go above target range sometimes, but left untreated it can cause health problems.
Let’s take a look at the signs and symptoms of hyperglycemia, and how you might lower your blood glucose back to a safe range.
What is hyperglycemia?
Hyperglycemia, or high blood sugar, is when too much glucose (sugar), usually from food, stays in the bloodstream, sending the blood glucose level above target range.
Insulin is the key hormone that allows glucose to be taken from the bloodstream to elsewhere in the body, where it can be used for energy.
People with type 1 diabetes take insulin because their body no longer produces it efficiently or at all.
People with type 2 diabetes may need to take insulin, if their bodies can’t make enough insulin, or cannot use the insulin it does make effectively.
It’s common for people with diabetes to experience episodes of hyperglycemia as well as hypoglycemia, which is when your blood glucose is too low.
Although frequent highs can be frustrating, maintaining good blood glucose control over the long term is what’s important.
Seek advice from your healthcare provider if you or the person you care for is experiencing frequent high blood glucose.
What is considered ‘high’ blood glucose?
For an adult with diabetes, a reading above 130 mg/dl before a meal, and above 180 mg/dl two hours after a meal could be considered a high blood glucose level.1
However, your target level may be different depending on your age, if pregnant and the type of diabetes you have1, so check with your healthcare provider for your personal blood glucose targets.
You can measure your blood glucose level by taking a reading with a blood glucose meter, or by tracking it with a continuous glucose monitor (CGM) or glucose sensor.
What causes hyperglycemia?
A common cause of hyperglycemia for people with type 1 or those with type 2 diabetes on insulin, is not dosing enough insulin for the carbohydrates in your food. But there are other reasons why your blood sugar levels may be too high.
Common factors include:2,3
- Missing an insulin dose completely
- Miss timed or miscalculated bolus
- Eating more carbohydrates than either the body or insulin (or both) can cope with
- Stress
- Illness/infection
- Over-treating hypoglycemia (low blood sugar)
- Experiencing dawn phenomenon (a surge of hormones that the body produces in the early morning hours around 4 or 5 am)
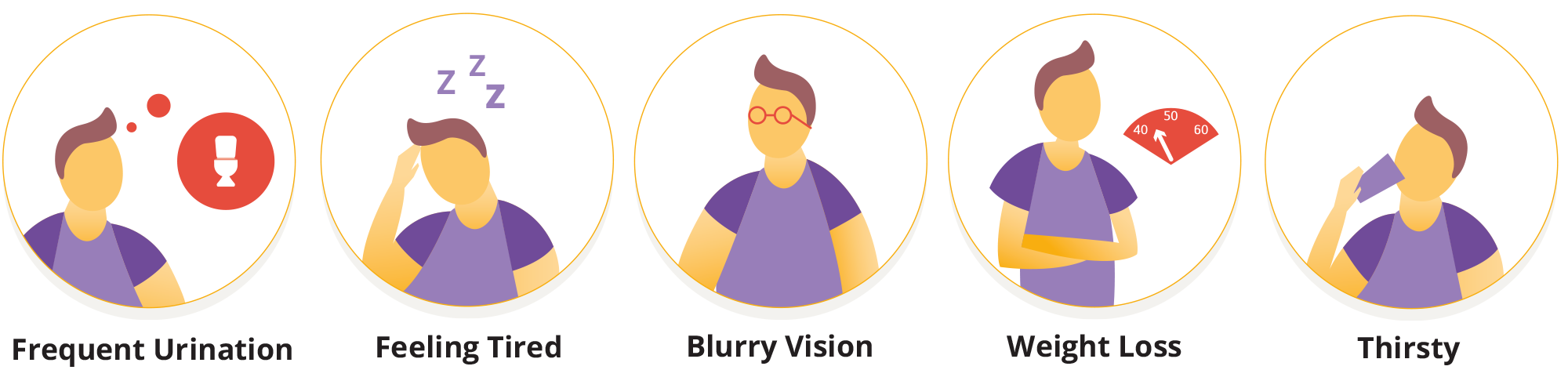
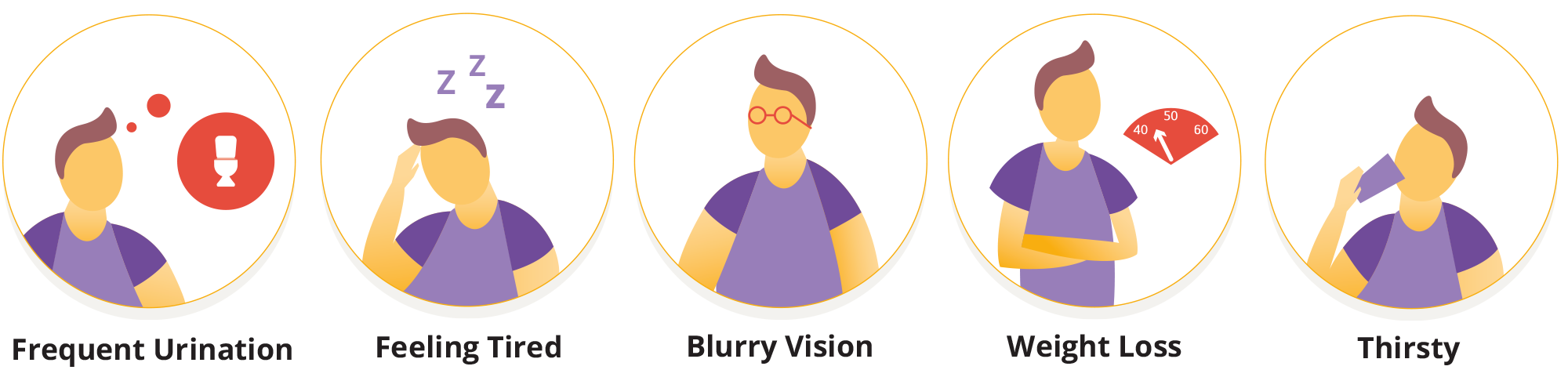
Signs and symptoms of hyperglycemia
If your blood glucose level is a little bit elevated you may not experience any symptoms, which is why regularly checking your blood glucose levels can help to prevent hyperglycemia.
As glucose levels continue to rise, you may experience some of the following symptoms:2,4
- Urinating (peeing) a lot
- Feeling tired or generally low in energy
- Blurred vision
- Weight loss
- Feeling thirsty
- Headaches
- Feeling sick or having stomach pains
- Having a strange taste in your mouth
Longer term symptoms of hyperglycemia include weight loss, yeast infections or thrush, cuts that won’t heal and other recurring infections.4
None of these symptoms are very nice to experience, so let’s look at how you might lower your glucose levels and get them back in range.
Lowering your blood sugar levels
As we mentioned, checking your blood glucose regularly with a blood glucose meter or with a glucose sensor can help you detect and treat hyperglycemia early. The best way to treat hyperglycemia as someone with type 1 diabetes is usually by taking insulin.
Your healthcare provider can help you determine how much insulin to take. They may provide you with your ‘correction factor’, or ‘insulin sensitivity factor’ which is the amount of insulin you need to bring down your blood glucose level by a certain amount.
Everybody’s insulin needs are different, and insulin also takes a little while to work, so it’s important to try and avoid ‘stacking’ doses too soon. This could lead to hypoglycemia, or low blood sugar.3
Outside of a specific episode of hyperglycemia, here are some ways that you can help to prevent them from occurring:3
- Being aware of your carbohydrate portions and how much insulin you need for carbohydrates. Carbs in foods raise your blood sugar more than proteins and fats. You can still eat carbs if you have diabetes. Counting carbs or being aware of carbs and portions is an important tool for managing blood sugar levels. Make sure to talk with your healthcare provider about the best way for you to manage your meals.
- Try to stay active. Everything from a short walk to a long bike ride will increase your insulin sensitivity in the long term and can help your body process sugar.
- Remember to take your insulin, even if you are ill or in a different routine.
- Check in with your emotional health as well as your physical health. Stress affects blood sugar levels, as does a lack of sleep. Focusing on your wellbeing can play an important role in blood glucose management.
The risks of hyperglycemia
Mild episodes of hyperglycemia (highs) aren’t too much cause for concern, and most of the time they can be treated with insulin if your blood sugar doesn’t return to a ‘normal’ level on its own.
If you’re experiencing hyperglycemia, drink plenty of water or sugar free fluids to prevent dehydration. Check your glucose levels frequently and if your readings are 240 mg/dL or more, it’s worth testing for ketones using a urine test strip or a blood ketone meter.3
High glucose levels left untreated over time can lead to long term health complications including damage to eyes, heart, kidneys, nerves and blood vessels. In extreme cases it could increase your risk of Diabetic Ketoacidosis or DKA, a serious and life-threatening condition.
In DKA, your body breaks down fat for energy because it doesn’t have enough insulin to use the sugar in your blood. This produces chemicals called ketones, which make your blood more acidic.
DKA is dangerous. Too much acid in your blood can make you pass out in a diabetic coma or even cause death.5
If you’re experiencing frequent or sustained hypers, speak with your healthcare team. You may need to adjust your insulin doses, insulin-to-carbohydrate ratios, or possibly other aspects of your management to help prevent the risk of long-term diabetes complications.
Continue reading:
Related Articles
References and Disclaimers
1- American Diabetes Association Professional Practice Committee; 6. Glycemic Goals and Hypoglycemia: Standards of Care in Diabetes—2025. Diabetes Care 1 January 2025; 48 (Supplement_1): S128–S145. https://doi.org/10.2337/dc25-S006
2- Hyperglycemia (High Blood Glucose) | American Diabetes Association
3- Manage Blood Sugar | Diabetes | CDC
4- Symptoms of Diabetes | Diabetes | CDC
5- About Diabetic Ketoacidosis | Diabetes | CDC
Explore our library for more articles on Type 1 Diabetes: https://www.omnipod.com/diabetes-hub/learning-center
These articles are not a replacement for medical advice or training. Please always speak to a qualified healthcare professional about your options.
The information and other content provided in this article, or in any linked materials, are not intended and should not be construed as medical advice, nor is the information a substitute for professional medical expertise or treatment. If you or any other person has a medical question or concern, you should consult with your healthcare provider. Never disregard professional medical advice or delay in seeking it because of something that have read on this blog or in any linked materials. If you think you may have a medical emergency, call your doctor or emergency services immediately. The opinions and views expressed on this blog and website have no relation to those of any academic, hospital, health practice or other institution.



