All about hyperglycemia
Hyperglycemia, or high blood glucose, can affect people living with type 1 diabetes. A person’s blood glucose will inevitably go out of range sometimes, but left untreated it can cause health problems.
Let’s take a look at the signs and symptoms of hyperglycemia, and how you might treat it to lower your blood glucose back to a safe range.
What is hyperglycemia?
Hyperglycemia, also known as hyperglycaemia or hyper, is when too much glucose (sugar), usually from food, stays in the bloodstream, sending the blood glucose level out of target range.
Insulin is the key hormone that allows glucose to be taken from the bloodstream to elsewhere in the body, where it can be used for energy.
People with type 1 diabetes take insulin because their body no longer produces it efficiently or at all.
It’s common for people with diabetes to experience episodes of hyperglycemia as well as hypoglycaemia, which is when your blood glucose is too low. You can check out the page on hypoglycemia here.
Although frequent hypers can be frustrating, maintaining good blood glucose control over the long term is what’s important.
Seek advice from your healthcare team if you or the person you care for is experiencing frequent hypers.
What is considered ‘high’ blood glucose?
For someone with diabetes, a reading above above 7mmol/l or 130 mg/dl before a meal, and above 8.5mmol/l or 155 mg/dl two hours after a meal could be considered a high blood glucose level1.
However your target level may be different depending on your age and the type of diabetes you have2, so check with your diabetes team for your personal blood glucose targets.
You can measure your blood glucose level by taking a finger prick test, or by tracking it with a continuous glucose monitor (CGM) or flash glucose sensor
If you’re looking for more information on CGMs (sensors), we’ve got you covered here.
What causes hyperglycemia?
A common cause of hyperglycemia for people with type 1 diabetes is not dosing enough insulin for the carbohydrates in your food. But there are other reasons why your blood sugar levels may be too high.
Common factors include1,3:
- Missing an insulin dose completely
- Eating more carbohydrates than either the body or insulin (or both) can cope with
- Stress
- Illness/infection
- Over-treating a hypo (low blood sugar)
- Hormonal changes
Certain types of exercise can raise blood sugar
Signs and symptoms of hyperglycemia
If your blood glucose level is a little bit elevated you may not experience any symptoms, which is why regularly checking your blood glucose levels can help to prevent hyperglycemia.
As glucose levels continue to rise, you may experience some of the following symptoms1,3 :
- Feeling thirsty
- Urinating (peeing) a lot
- Feeling tired or generally low in energy
- Headaches
- Blurred vision
- Feeling sick or having stomach pains
- Having a strange taste in your mouth
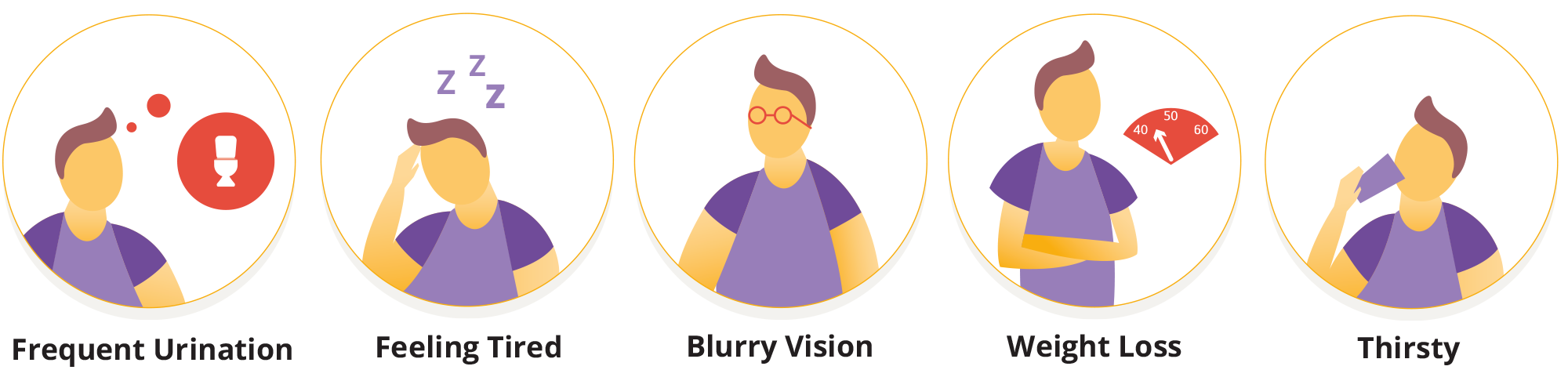
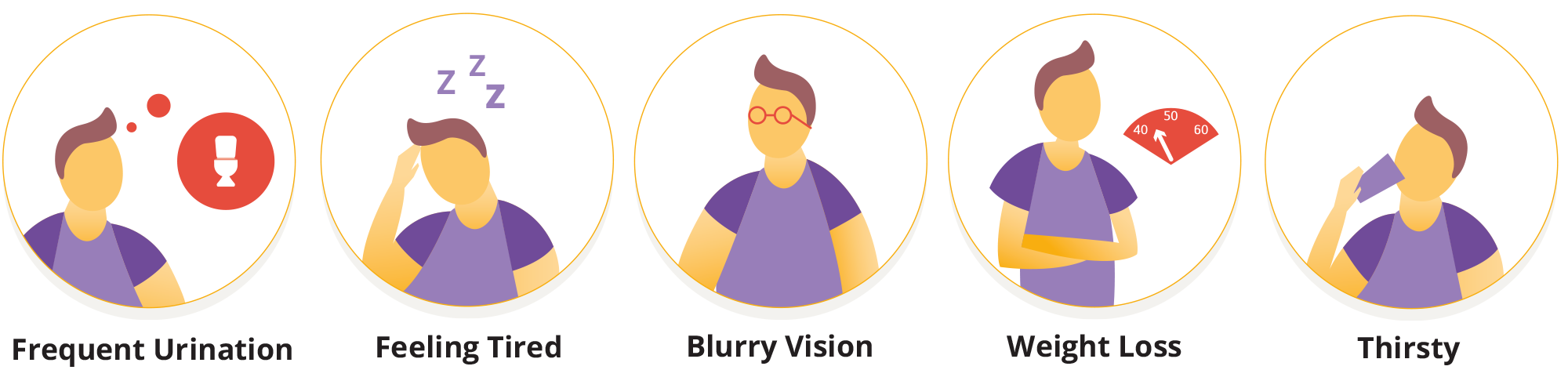
Longer term symptoms of hyperglycaemia include weight loss, yeast infections or thrush, cuts that won’t heal and other recurring infections.
None of these symptoms are very nice to experience, so let’s look at how you might lower your glucose levels and get them back in range.
Lowering your blood sugar levels
As we mentioned, checking your blood glucose regularly via a finger prick test or with a glucose sensor can help you detect and treat hyperglycemia early. The best way to treat hyperglycemia as someone with type 1 diabetes is usually by taking insulin.
Your doctor or diabetes team can help you with your ‘correction factor’, or ‘insulin sensitivity factor’ which is the amount of insulin you need to bring down your blood glucose level by a certain amount.
Everybody’s insulin needs are different, and insulin also takes a little while to work, so it’s important to try and avoid ‘stacking’. This is when you take multiple doses of insulin in a short period of time, which could lead to hypoglycaemia, or low blood sugar.3
Outside of a specific episode of hyperglycemia, here are some ways that you can help to prevent them from occurring1:
- Being aware of your carbohydrate portions and how much insulin you need per 10g of carbohydrate. A carb-counting course can help you understand this in more detail - ask your healthcare team for more information.
- Try to stay active. Everything from a short walk to a long bike ride will increase your insulin sensitivity in the long term, and can help your body process sugar.
- Remember to take your insulin, even if you are ill or in a different routine.
- Check in with your emotional health as well as your physical health . Stress affects blood sugar levels, as does a lack of sleep. Focusing on your wellbeing can play an important role in blood glucose management.
The risks of hyperglycemia
Mild episodes of hyperglycemia (hypers) aren’t too much cause for concern, and most of the time they can be treated with insulin if your blood sugar doesn’t return to a ‘normal’ level on its own.
If you’re experiencing hyperglycemia, drink plenty of water or sugar free fluids to prevent dehydration. Check your glucose levels frequently and if your readings are 15 mmol/l or more, it’s worth testing for ketones using a urine test strip or a blood ketone meter1.
Sustained periods of high glucose can become dangerous if left untreated, and you could be at risk of developing Diabetic Ketoacidosis, or DKA.


In DKA, your body breaks down fat for energy because it doesn’t have enough insulin to use the sugar in your blood. This produces chemicals called ketones, which make your blood more acidic.
DKA is dangerous. Too much acid in your blood can make you pass out in a diabetic coma or even cause death3.
If you’re experiencing frequent or sustained hypers, have a chat with your healthcare team. You may need to adjust your insulin doses, insulin to carbohydrate ratios, or possibly other aspects of your management in order to help prevent the risk of long-term diabetes complications.
So that’s hyperglycemia explained.
You may also want to take a closer look at hypoglycaemia, also known as low blood sugar.
1 https://www.diabetes.org.uk/guide-to-diabetes/complications/hypers
2 https://www.nhs.uk/conditions/high-blood-sugar-hyperglycaemia/
3 https://www.jdrf.org/t1d-resources/about/symptoms/blood-sugar/high/
Explore our library for more articles on Type 1 Diabetes.
Related Articles
References and Disclaimers
These modules are not a replacement for medical advice or training. Please always speak to a qualified healthcare professional about your options.



