Insulin Pump Therapy for Children with Type 1 Diabetes
Everyone who has type 1 diabetes, including children and adults, must take insulin to replace the insulin their body no longer makes. In addition, many people who have type 2 diabetes need to take insulin to manage their glucose levels. Today there are several types of insulin, two common types are rapid-acting and long-acting insulin. Children with type 1 diabetes may take multiple daily injections [MDI], using rapid and long-acting insulin, or use an insulin pump. Children who use insulin pumps only use rapid-acting insulin in the pump.
The use of insulin pump therapy can make taking insulin easier and more convenient. Insulin pumps deliver small and precise amounts of insulin. In addition, insulin pump therapy can help children and their caregivers more easily manage glucose levels with their varied eating and physical activity schedules. This article aims to help children with type 1 diabetes and their caregivers learn the basics about insulin pump therapy to help determine if it is right for them. For caregivers of children with type 2 diabetes, you can learn about the benefits of insulin pump therapy for type 2 diabetes here.
What are the basics of insulin pump therapy for type 1 diabetes?
An insulin pump delivers insulin, just like an injection, right under the skin (known as subcutaneously). But what is different is that the insulin pump user gets their insulin continuously all day long. The insulin is delivered through a narrow tube that is placed by the user with a thin, short needle just under the skin. Insulin pump therapy uses just one type of insulin, rapid-acting. The pump delivers insulin as it is directed by the user’s settings in two ways – basal and bolus.1 Settings are prescribed and guided by the person’s diabetes healthcare providers.
What do the terms basal and bolus mean?
Basal Insulin
Basal insulin is also known as background insulin. The pump delivers small amounts of rapid acting insulin continuously and automatically throughout the day at a rate determined by your provider.2 This is called the basal rate and provides the insulin a person needs to keep glucose levels within their target range in between meals and overnight. It replaces the need for long-acting insulin.
A benefit of insulin pump therapy is that the basal rate can be adjusted based on the user’s basal insulin needs. The user can set different rates for different time segments of the day when they need more or less insulin. For example, overnight they may need a different rate of insulin to help them wake up in range. Another benefit of an insulin pump is that the user can temporarily set their basal rate to deliver more or less insulin for a short period of time. This comes in handy for exercise, when less basal insulin might be needed and sick days, when more basal insulin might be needed.
Bolus Insulin
Bolus insulin is the insulin that is delivered for meals or to correct a high blood glucose.2 The user will prompt the pump to deliver the bolus insulin dose when needed. Depending on the functionalities of the pump, the user can choose to take the bolus dose all at once or to extend all or part of it over a number of hours. This is often used for foods or meals that are elevating blood glucose levels longer than usual.
When can a child with type 1 diabetes start insulin pump therapy?
A child with type 1 diabetes can successfully start insulin pump therapy at any point of their life with diabetes, including at the time of diagnosis.1 If insulin pump therapy is something that caregivers and loved ones believe would be of benefit to a child, it is important to discuss this with the child’s diabetes healthcare providers.
How many insulin pumps are available and how are they tested?
Today there are several companies that manufacture insulin pumps around the globe. Prior to being made available for purchase, these insulin delivery devices are thoroughly tested by the manufacturer and reviewed by regulatory authorities, such as the Food and Drug Administration (FDA) in the U.S. Once a device is given clearance, it must be prescribed to the child with type 1 diabetes by their healthcare provider. Along with the prescription, the healthcare provider gives specific instructions for how the insulin pump should be programmed.
After receiving the pump, the child with type 1 diabetes and their caregivers are taught how to use it. This is done by a healthcare provider, typically a Certified Diabetes Care and Education Specialist (CDCES), that is also a Certified Pump Trainer (CPT) for the chosen pump. A child with type 1 diabetes and their caregivers are instructed on the basics of insulin pump therapy and the specifics about their particular pump. Device manufacturers can also help people troubleshoot when difficulties arise with the systems.1
What are the two main types of insulin pumps?
A traditional insulin pump includes an infusion set, tubing and the insulin pump itself. The infusion set includes a smaller tube, called a cannula, that the user inserts under the skin. The infusion set can be placed on the body almost anywhere insulin can be injected such as the abdomen, lower back, leg, arm or buttock. The insulin pump itself, which holds the insulin and is the interface to deliver a bolus or change settings, is worn on the body—e.g., clipped at the waist, in a woman’s bra, in a pouch around the waist or in a pocket.


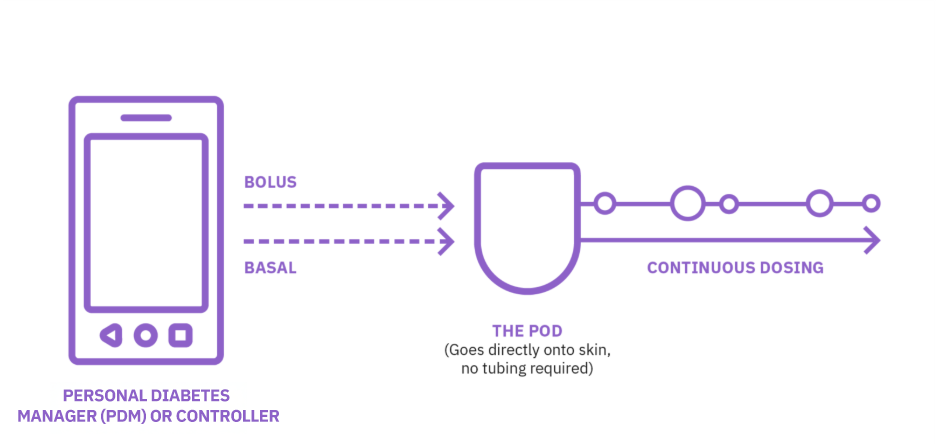
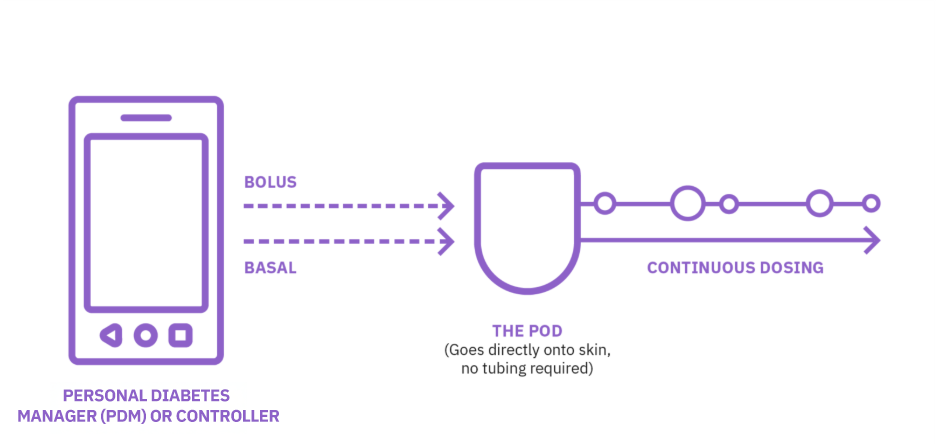
The other type of insulin pump is a tubeless pump. In a tubeless system, such as Omnipod® 5, a Pod is filled with insulin and worn directly on the body almost anywhere insulin can be injected, similar to the tubed pump. The Pod contains a cannula within the Pod and is automatically inserted under the skin. The other piece of the tubeless system is the controller that is used to direct the actions of the Pod. A big benefit of this system is that this controller only needs to be near the user to deliver a bolus or change settings.* Therefore, the controller device does not need to be carried on the body at all times.
The insulin pump user typically needs to change their infusion set and pump tubing or Pod site every two or three days. Another benefit of a tubeless insulin pump is not having to deal with the inconveniences and challenges of the long tubing becoming snagged or tangled, which can pull out the infusion set.
Insulin pumps have been available for four decades.1,3 Through the years insulin pumps have gotten much smaller and easier to use. In addition, new features have been added to make insulin delivery easier and more convenient as well as features that can potentially reduce hypoglycemia (low glucose levels) and hyperglycemia (high glucose levels). Such as the ability to consider active insulin from a previous bolus also called ‘insulin on board’.
Insulin pumps give more precise insulin doses compared to MDI such as bolus and basal increments as low as 0.025u. Over the last several years, as continuous glucose monitoring (CGM) has become more available to people with diabetes, several insulin pumps can integrate and provide CGM data to the user and their healthcare provider for more precise and easier management.
Are there additional benefits of insulin pump therapy for a child with type 1 diabetes?
Yes, quite a few in fact!2-4
Fewer calculations and less math for the child’s caregiver to do to determine how much bolus insulin to take to cover food (meals, snacks) and to account for high or low glucose levels
Greater personalization upon which to base optimal bolus doses. The individual insulin to carbohydrate ratio, insulin correction factor, duration of insulin action, and more, are preset with a healthcare provider’s guidance. (These can be changed as needed.)
Easier to deal with the varied and irregular schedule of a child’s life whether at pre-school, school, on the playground or at play with siblings, friends, or others.
Fewer incidences of hypoglycemia (low blood glucose)5
Set reminders and alerts to take your bolus insulin doses, check your glucose level, and change your insulin site or Pod.
Access by the user and their healthcare providers to all the insulin pump data and reports.
Ability to take small and precise doses of both basal and bolus insulin (if needed). Young children with type 1 diabetes typically need smaller doses than adults.
Fewer diabetes care supplies to carry because the user is wearing their insulin. However, it is always recommended to carry backup supplies.
Is insulin pump therapy right for my child with type 1 diabetes?
- Choosing to start insulin pump therapy to manage a child with type 1 diabetes is a decision that should be made in concert with a diabetes healthcare provider. Insulin pump therapy may be a good option for a child with type 1 diabetes if the child:2,3
- needs and wants an easier way to deliver insulin
- has an unpredictable schedule that may result in varied insulin needs
- needs substantial amounts of basal and/or bolus insulin
- has higher and/or lower basal insulin needs during the day and/or night
- participates in athletics or exercise
- wants to give insulin more discreetly
Is an insulin pump covered by healthcare plans?
If your child with type 1 diabetes has private health insurance, insulin pump therapy will typically be covered. Some people with other forms of state and federal government health coverage (Medicaid and Medicare) may cover insulin pump therapy. The tubeless pump (Omnipod) may also be available through a pharmacy or Medicare Part D plan. The best way to learn about whether the health plan the child is covered under will cover the insulin pump that you want is to contact the insulin pump company. Their staff will help you determine your coverage.
Learn More about the Benefits of Insulin Pump Therapy
Learn more by reading real life stories from people wearing pump therapy systems. Discover how insulin pump therapy is making a world of difference in their lives.
Continue Reading
Related Articles
Other topics
References and Disclaimers
1: American Diabetes Association Professional Practice Committee. 7. Diabetes technology: Standards of Care in Diabetes—2025. Diabetes Care 2025;48(Suppl. 1):S146–S166
2: Walsh J, Roberts R. Pumping insulin, 5th ed.Torrey Pines Press. 2012.
3: Sikes KA, Weyman K. Diabetes and the use of insulin pumps. Endocrin Advisor. https://www.endocrinologyadvisor.com/home/decision-support-in-medicine/endocrinology-metabolism/diabetes-and-the-use-of-insulin-pumps/. Accessed March 3, 2021.
4: Scheiner G. Think like a pancreas. 3rd ed. Hachette Books. 2020.
5: Diabetes Spectrum 2019 Aug; 32(3): 194-204
These modules are not a replacement for medical advice or training. Please always speak to a qualified healthcare professional about your options.
The information and other content provided in this article, or in any linked materials, are not intended and should not be construed as medical advice, nor is the information a substitute for professional medical expertise or treatment. If you or any other person has a medical question or concern, you should consult with your healthcare provider. Never disregard professional medical advice or delay in seeking it because of something that have read on this blog or in any linked materials. If you think you may have a medical emergency, call your doctor or emergency services immediately. The opinions and views expressed on this blog and website have no relation to those of any academic, hospital, health practice or other institution.



