Understanding Flash Glucose Monitoring and Continuous Glucose Monitoring
Continuous glucose monitors (CGM) and flash glucose sensors (FGS) are small wearable devices that allow people with type 1 diabetes to monitor glucose levels without the use of finger prick testing*.
CGMs and FGSs have revolutionised diabetes management because the large amount of data they provide gives you a much clearer picture of glucose levels.
What is a flash glucose sensor or continuous glucose monitor?
Flash glucose sensors and continuous glucose monitors allow users to check their sugar levels without having to use finger pricks+.
A continuous glucose monitor or flash glucose sensor provides hundreds of real-time glucose readings per day, wirelessly sent to your phone or a separate receiver.
This offers a continuous update of your glucose levels, giving you invaluable insights into diabetes management and how the body is responding to food and daily activity.
They can generally be worn when bathing, showering, or swimming but always check with the different manufacturer’s recommendations. The sensor must be replaced every 6 to 15 days depending on the system. This is carried out by the user or their caregiver.




How does a flash glucose sensor or CGM work?
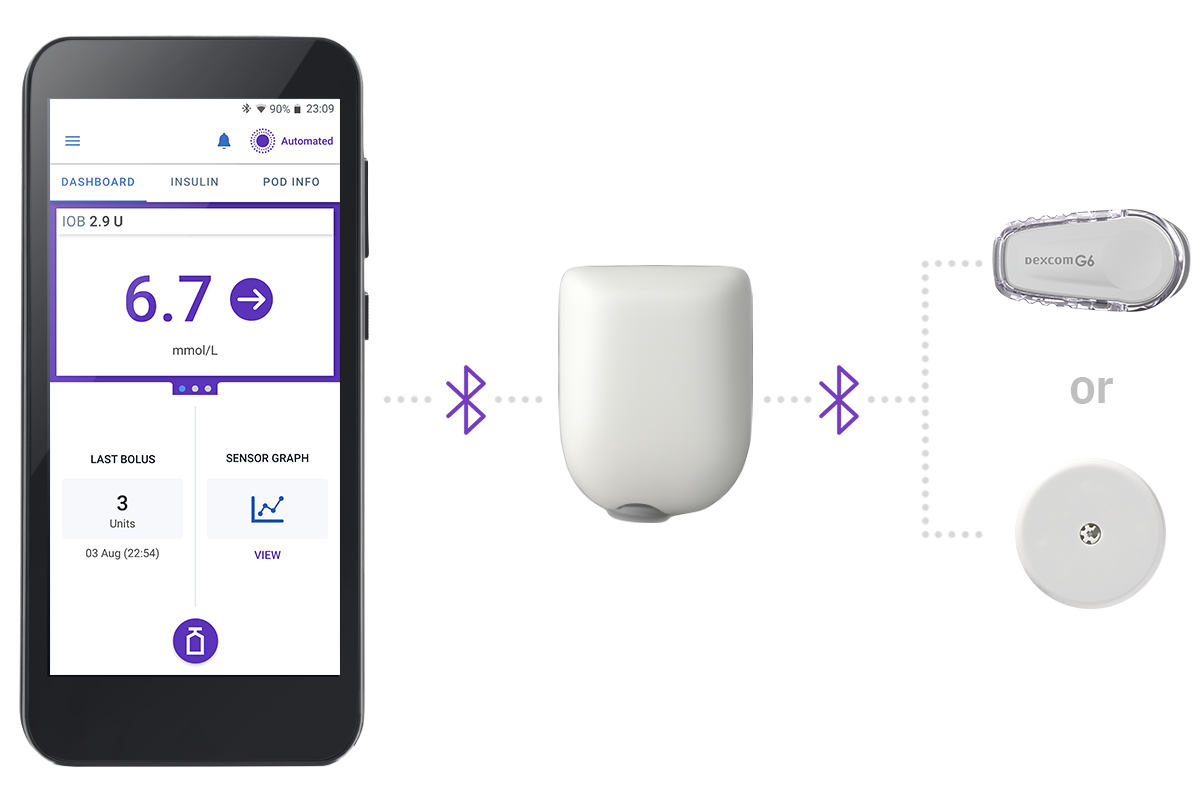
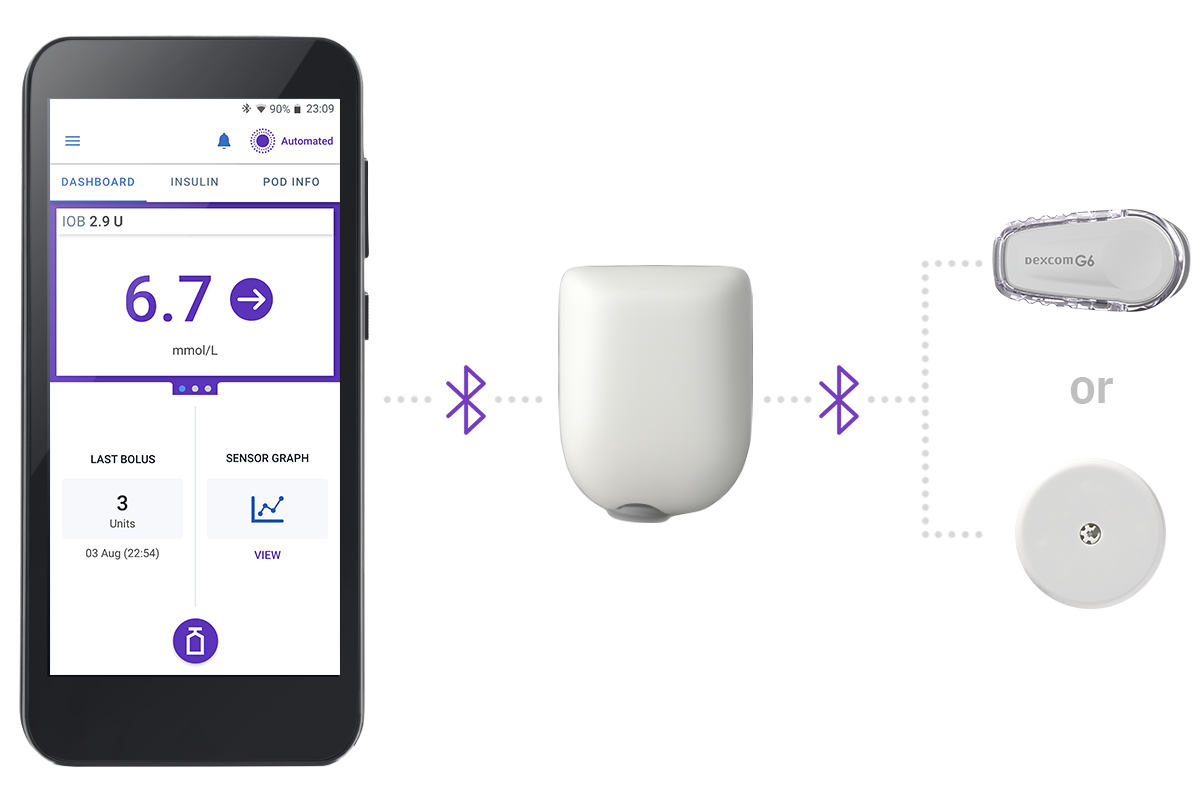
A CGM or flash glucose sensor usually works as a three-part team, 24 hours a day:
- The sensor sticks to the body using an adhesive patch, with a thin filament inserted under the skin. Every few minutes it takes a reading from ‘interstitial fluid’, which is different from the glucose reading taken with finger prick testing.
- The transmitter which fits onto the sensor or is built into the sensor. It communicates the reading wirelessly to…
- The smartphone app or receiver where you can easily get your current glucose reading and track the direction of your glucose levels, as well as trends over time.
You may still need to occasionally finger prick, for example, if what you’re feeling doesn’t match what your reading says or if you want to double check before treating a high or low sensor reading.
This is why it’s important that you still get your diabetes kit on prescription, including your blood glucose meter, to allow you to do finger prick checks1.
CGM and FGS readings are some minutes behind the current blood glucose levels, and therefore readings can differ from a finger prick test, especially if glucose levels are falling or rising rapidly.
What’s the difference between a flash glucose sensor and a continuous glucose monitor?
A CGM is a real-time continuous glucose monitor (rtCGM), while a Flash Glucose Sensor is what’s called an intermittently-scanned continuous glucose monitor (isCGM).
With an isCGM, you need to wave (or scan) a device over the sensor to get the glucose reading. This can be done over clothes, including thick clothing like coats.
Unlike an isCGM, an rtCGM automatically transmits the readings, via Bluetooth, to a receiver or smartphone every few minutes without any need for scanning.


Key benefits of continuous glucose monitors and flash glucose sensors
- You can check your glucose levels very quickly, on the move.
- Data shows clearly whether glucose levels are high, low or in range.
- In addition, trend arrows show whether glucose levels are rising, falling, or stable.
- Some sensors can even send this data to a smartwatch.
- The data can also be sent to another device, for example a parent or partner’s phone, or your healthcare team ahead of your appointments.
- The large quantities of data can help to spot patterns in glucose behaviour, like spiking after certain foods, at certain times of the day or during exercise.
- Many sensors use alarms to alert you when your blood glucose is too high or too low. This can be particularly useful at night.
How does a FGS or CGM help with type 1 diabetes management?
The glucose information and trends give someone living with diabetes a greater picture of what their glucose levels are doing at any given time of the day.
This information can be used to help inform treatment decisions - for example around when waking, eating, or during exercise.
Some sensors will also alert you when your glucose is running high or low, or even predict hypoglycaemia in advance. This feature can help give greater peace of mind when it comes to hypoglycaemia or hyperglycaemia.
Research suggests that continuous glucose monitoring can help people with type 1 diabetes improve their time in range, as well as reducing their HbA1c without increasing the risk of hypoglycaemia.2, 3
Can I use a glucose monitor alongside a Pump?
The short answer is yes.
For example, any glucose monitor can be used alongside your Omnipod DASH® System to monitor your glucose levels. The user will manually input these readings into the Personal Diabetes Manager (PDM) for a meal or correction bolus.
The Omnipod® 5 System currently integrates with Dexcom G6 CGM to enable Automated Insulin Delivery (AID).
Real-time CGMs are an essential part of Automated Insulin Delivery (AID) or Hybrid Closed Loop (HCL) Systems, like Omnipod 5.
The glucose readings from the rtCGM are sent wirelessly to the Pump or Pod, where an in-built algorithm continuously adapts to automatically deliver basal insulin according to your personal needs. This may help to control blood glucose levels, reduce hypoglycaemia, and increase time in range4. We will cover this in much more detail in our What is Automated Insulin Delivery module.
Is Omnipod 5 right for me?
Find out more about the Omnipod 5 Automated Insulin Delivery System and how it works together with Dexcom G6 to incorporate your rtCGM data and trends to automatically adjust insulin delivery.
Frequently Asked Questions about CGMs
How does a continuous glucose monitor differ from finger prick testing?
How often do you have to change a flash or CGM sensor?
Where can I wear a flash or CGM sensor?
Can I share my glucose data with friends and family?
What is the Omnipod 5 Automated Insulin Delivery System?
Continue reading:
Automated Insulin Delivery (AID) is revolutionising the way people manage their type 1 diabetes. Let’s find out what it’s all about.
Related Articles
Other topics
References and Disclaimers
1 https://www.diabetes.org.uk/guide-to-diabetes/diabetes-technology/flash-glucose-monitors-and-continuous-glucose-monitors
2 Beck RW, Riddlesworth T, Ruedy K, Ahmann A, Bergenstal R, Haller S, Kollman C, Kruger D, McGill JB, Polonsky W, Toschi E, Wolpert H, Price D; DIAMOND Study Group. Effect of Continuous Glucose Monitoring on Glycemic Control in Adults With Type 1 Diabetes Using Insulin Injections: The DIAMOND Randomized Clinical Trial. JAMA. 2017 Jan 24;317(4):371-378. doi: 10.1001/jama.2016.19975. PMID: 28118453.
3 Welsh JB, Gao P, Derdzinski M, Puhr S, Johnson TK, Walker TC, Graham C. Accuracy, Utilization, and Effectiveness Comparisons of Different Continuous Glucose Monitoring Systems. Diabetes Technol Ther. 2019 Mar;21(3):128-132. doi: 10.1089/dia.2018.0374. Epub 2019 Jan 25. PMID: 30681379; PMCID: PMC6434583.
These modules are not a replacement for medical advice or training. Please always speak to a qualified healthcare professional about your options.
The information and other content provided in this article, or in any linked materials, are not intended and should not be construed as medical advice, nor is the information a substitute for professional medical expertise or treatment. If you or any other person has a medical question or concern, you should consult with your healthcare provider. Never disregard professional medical advice or delay in seeking it because of something that have read on this blog or in any linked materials. If you think you may have a medical emergency, call your doctor or emergency services immediately. The opinions and views expressed on this blog and website have no relation to those of any academic, hospital, health practice or other institution.



