Omnipod® 5 Aligns with ADA 2026 Standards of Care
Omnipod 5 is a tubeless AID system, providing automated insulin delivery every 5 minutes, based on current and predicted glucose levels, to proactively help to correct hyperglycemia, and help protect from hypoglycemia.
Earlier & broader access
- Omnipod 5’s pharmacy benefit and access through Medicare Part D means no C-peptide required, reduced paperwork burden and ease of issuing prescriptions
- RADIANT2, a randomized control trial showed successful direct transition for those with type 1 diabetes on MDI to Omnipod 5, resulting in 22% increased TIR, with no increase in hypoglycemia.
- SECURE-T2D3 showed A1c reductions, and more Time in Range (TIR), without more hypoglycemia in a diverse population with type 2 diabetes, regardless of patient’s race, ethnicity, GLP-1 use, and carbohydrate counting status.
Person-centric Individualization – Omnipod 5’s tubeless simplicity, adjustable Glucose Targets, compatibility with leading CGM sensors, and smartphone control allow customization to meet patient’s needs and preferences.
Education and follow-up – Omnipod 5’s data is automatically collected to the cloud, without burden from the user, allowing healthcare professionals to access their patient's data more efficiently to optimize diabetes management. Clinical tools like those created by the PANTHER Program give providers standardized guidance4.
Putting Guidelines into Practice: The Role of AID and Omnipod 5
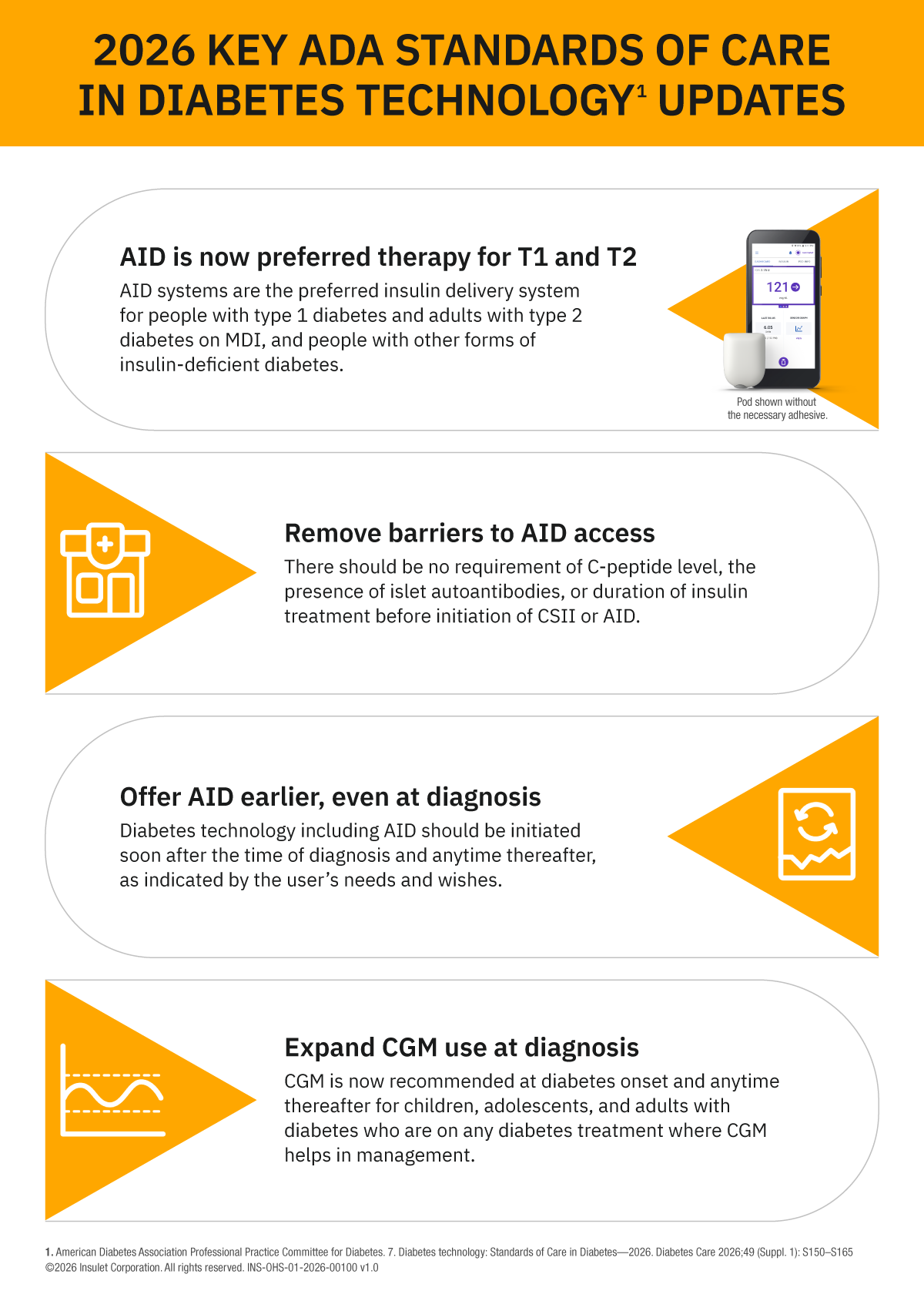
The 2026 ADA Standards of Care make it clear: Automated Insulin Delivery is no longer optional—it’s the preferred approach for insulin delivery in both type 1 and type 2 diabetes. This shift reflects robust evidence and a commitment to improving outcomes and reducing burden for people living with diabetes.
- Act early—introduce AID without unnecessary prerequisites.
- Personalize care—choose devices that fit patient lifestyles and goals.
- Support success—pair technology with education and ongoing follow-up.
Omnipod 5 stands at the forefront of this evolution, offering tubeless simplicity, and proven results from real-world data and the RADIANT and SECURE-T2D studies.
By embracing these recommendations and leveraging innovations like Omnipod 5, clinicians can help transform diabetes management—delivering better control, greater flexibility, and improved quality of life for every patient who needs insulin.
1. American Diabetes Association Professional Practice Committee for Diabetes. 7. Diabetes technology: Standards of Care in Diabetes—2026. Diabetes Care 2026;49(Suppl. 1): S150–S165
2. A 13-week randomized, parallel-group clinical trial conducted among 188 participants (age 4- 70) [51% HbA1c≥ 8% (64 mmol/mol)] with type 1 diabetes in France, Belgium, and the U.K., comparing the safety and effectiveness of the Omnipod 5 System versus multiple daily injections with CGM. Time in range (70-180 mg/dL or 3.9-10mmol/L) with OP5 improved by 22% (43% MDI vs. 65% OP5, p<0.001). Time below range (<70 mg/dL or <3.9mmol/L) with OP5 was non- inferior to MDI (2.27% MDI vs. 2.56%, p=0.2). Data on file. 2025. RF-042025-00015.
3. Pasquel FJ, et al. JAMA Network Open (2025). Prospective pivotal trial in 305 participants with T2D aged 18-75 yrs. Study included a 14-day standard therapy (ST) phase followed by a 13-week Omnipod 5 hybrid closed-loop phase. Mean time in range (70-180 mg/dL): ST vs. 13-week Omnipod 5: 45% vs. 66%, P<0.001. Mean HbA1c: ST vs. 13-week Omnipod 5: 8.2% vs. 7.4%, P<0.001. Mean time <70 mg/dL as measured by CGM: standard therapy = 0.2%, 3-mo Omnipod 5 = 0.2%. In a subgroup analysis of 164 participants who used GLP-1 RA mean HbA1c: baseline vs. 13-week Omnipod 5: 8.1% vs. 7.3%; compared to 132 participants who did not use GLP-1 RA mean HbA1c: baseline vs. 13-week Omnipod 5: 8.4% vs. 7.5% Interaction p-value p= 0.5
4. PANTHER Program. PANTHERTOOL for Omnipod 5 Automated Insulin Delivery System. Accessed on January 9, 2026. Available at: https://www.pantherprogram.org/omnipod-5
INS-OHS-12-2025-00238 v2.0