Mainstreaming and Mechanizing Menstruation & T1D
I remember waiting in the school office. I sat there with my underwear secretly stuffed with toilet paper to hide the evidence. My dad was on his way.
It was towards the end of my grade 8 year.
As far as I knew, I was the last girl in our grade to get my period.
For me, the stigma attached to menstruation is bizarre. Not just because it is part of our biology, but because it was always an open discussion in our house.
Still, I was a little afraid and nervous; this was unfamiliar territory for me. And my dad was about to guide me through it.
Together we sat on the edge of my bed. My dad had a pair of my mom’s underwear and a sanitary pad. He pulled the underwear over his dress pants and opened the pad, peeled off the paper to expose the adhesive, then attached it to the inside of the underwear.
I then went to bathroom and repeated the steps myself.
I was almost fourteen and this was my first period.
My type 1 diabetes diagnosis would come four years later. But it would be a quarter century later when I discovered the inner workings of my cycle and what it did/how it affected my type 1 diabetes.
To say I had a challenging time finding information about the relationship between the two over the years would be an understatement. There is not much data and information available. As normal as it is, menstruation remains stigmatized around the world.
I would be in my mid-thirties when my suspicions about my blood glucose levels and menstruation were confirmed, and I began to see the correlation between my monthly cycle and shifts in my blood glucose levels. It would take another couple of years before I was empowered using my Omnipod® insulin pump to fine tune my inner workings and make changes that would help me be more successful during those monthly shifts.
Menstruation remains something people are hesitant to talk about. Even in preparation for this blog I found it difficult to gather information about T1D and periods.
Periods are still taboo.
Thanks to the use of social media, attitudes are changing but we still have miles to go to break the taboo.
A Brief Step Back in Time
Menstruation has been the stuff of mystery for centuries.
There are all sorts of strange myths and beliefs surrounding menstruation.
From ancient times to the start of the medieval era, menstrual blood was believed to have curative capabilities. It was thought to fix sagging breasts and even cure leprosy. A lot of the shame surrounding periods stems from the medieval era.
Equally strange are the beliefs that periods could alter the weather and destroy crops. In modern times, it is still believed that a menstruating person can contaminate food or even make others sick just by stepping into a room.
Somewhere in our history, period blood was placed into the “gross” category along with fecal waste and urine rather than classified as a secretion like other blood or saliva.
Clean up in Aisle T1D!
Most young people do not have an accurate understanding of menstruation, let alone how it can impact their diabetes. Educating and making such information more accessible will build confidence. Not just in a “normalize periods” way but in a “better your diabetes management” way.
Menstruation means hormonal changes and these can affect how your body functions, so it can present a unique set of challenges for those living with type 1 diabetes.
Between my first period and my T1D diagnosis I saw several specialists because my menstrual cycles were consistently irregular. After several tests, I was told I had traits related to polycystic ovary syndrome (PCOS). This is something I would later learn is frequently seen in women with type 1 diabetes and can contribute to insulin resistance during menstruation.
My menstrual struggles continued beyond my T1D diagnosis and into my mid-twenties. I again saw numerous specialists and had several exploratory surgeries. Yet no one, not even my many different endocrinologists during those times, ever mentioned my diabetes.
Looking to connect with the T1D community? Start by joining the Pod Squad today!
People living with type 1 are so conditioned to think that irregularities in our blood glucose are our fault that it never really occurred to me that monthly changes in my hormone levels were the likely culprit of fluctuations in my blood glucose levels.
Increased progesterone levels midway through your cycle can cause increased insulin resistance. This means that even though you are doing EVERYTHING humanly possible, employing every tool in your diabetes arsenal, you may still see spikes in your blood sugar before you menstruate.
And that can be a frustrating monthly blow.
Especially if you consider just how much of your life is occupied by menstruation and T1D. You will spend a decade of your life on your period, from your first cycle to menopause. Of course, not everyone’s cycle is the same, so length of cycle and the number of periods will differ over a person’s lifetime.
On average, people living with diabetes spend 14+ hours weekly managing their T1D. For me, should I live into my late seventies, this means I will spend 5+ years of my life managing my diabetes. When you add it all up, that is a tremendous amount of time in life lost to or absorbed by things like menstruation and chronic illness.
Another thing that cleared up for me (literally) once I started tracking my periods and using an insulin pump were recurring yeast infections. I knew people living with diabetes were more susceptible to infection, but I did not realize that included yeast infections.
While not all high glucose levels cause yeast infections, the excess of sugar in your blood makes you more prone to a yeast infection because that yeast feeds on sugar.
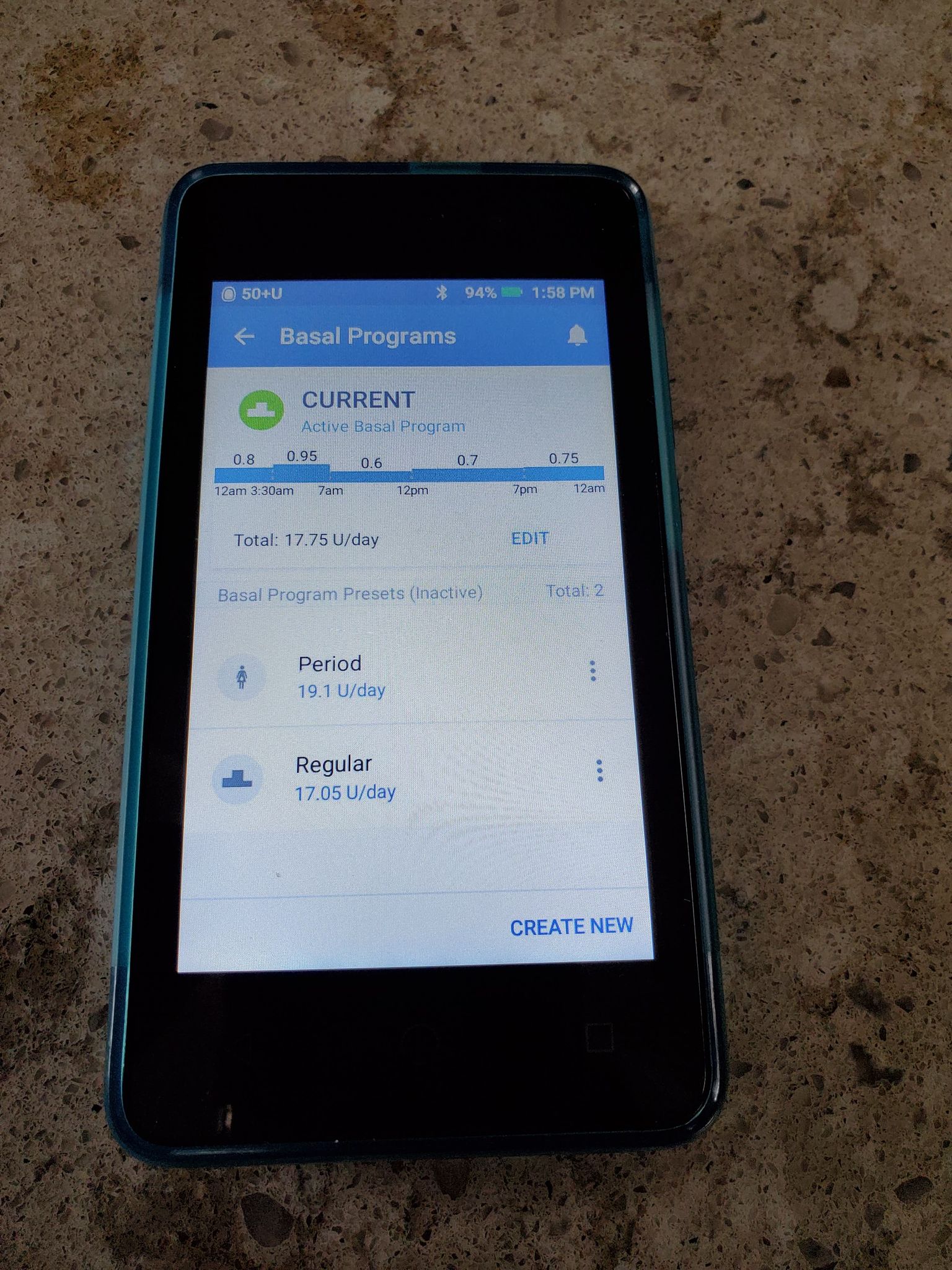
Before switching to an insulin pump, those elevated pre-cycle blood glucose levels of mine often resulted in an infection during menstruation. Being able to set a basal program specifically for my cycle has made a tremendous difference in my management, and my overall health and well-being. It’s important to discuss what would work best for you with your diabetes team.
Another challenge with menstruation and T1D, that I only learned about recently, is that periods are typically worse when it is cold. They are likely to be heavier and longer than your normal cycle during the winter/in cold climates. Even symptomatic pain can be elongated.
The Other “M” Word
My own unique health journey temporarily threw me into pre/early menopause. It was that event, and those it triggered, that found me researching about menstruation/menopause.
In doing so I discovered things about menstruation, menopause and living with type 1 diabetes, things no healthcare professional had ever shared with me.
Nearing 40 years of age, I have learned so many things about my period and living with diabetes that would have helped during my late teenage and young adult years.
I also learned that most teenagers and young adults living with type 1 experience irregular cycles. And while it is unknown why, knowing that would have relieved me of stress in my early twenties.
Living with T1D also means I may experience menopause sooner than someone without diabetes.
Uncovering all this new knowledge prompted me to do even more investigating into my cycle to better help me with my diabetes management.
Mechanized Menstruation
While we wait to normalize talking about periods, technology has managed to evolve and brought us things like period tracking apps. I find these so helpful because I can now track when my PMS symptoms should hit each month and that allows me to take steps to minimize their impact.
Being able to employ the basal presets on my Omnipod DASH® PDM means I am better prepared to manage those inevitable blood glucose fluctuations. I am so grateful for the ability to do that because it takes away the stress that comes along with my monthly cycle.
The truth is it should not be hard to find information about periods or living with a chronic illness like type 1 diabetes and its impact on menstruation. Period taboos are holding us back and emphasize the need to educate and empower those who menstruate.
Language can also be problematic and create stigma if we do not use the actual word. There are over 5,000 euphemisms for periods/menstruation, in approximately ten different languages around the globe. The avoidance of proper terminology can lead to misunderstanding and damaging misconceptions.
A lot of what we know about menstruation is only just now emerging, even though menstruation has occurred in humans since before our evolution was complete. Thankfully, we are progressing and there are studies underway looking at menstruation and diabetes.
Yet, normal as it is, menstruation remains stigmatized around the world. We need to raise awareness and highlight the biology of periods, so the mythology becomes non-existent.
I am grateful to have had opportunities (including this one) to share my experiences, and data, to help shine light on the topic.