Omnipod® 5 Free Trial, Copay Cards, and Financial Assistance
Omnipod® 5 is the only tubeless AID in the US available through the pharmacy, without going through DME. Many patients can start today.* Now you can even let your patients try it for free for 10 days.


We’re Committed to Patient Access
- Omnipod 5 has over 90% insurance coverage, representing over 300 million covered lives in the US!1
- The majority of Omnipod 5 customers pay $50 or less per month.2
- More than half of covered Omnipod 5 scripts are filled within 24 hours through the pharmacy.3
Our 10-Day Free Trial† and Copay Card§
As part of our mission to simplify diabetes, we seek to ease the burdens of access to our products. For patients hesitant to switch or start therapy, or patients who have financial concerns, but want to start on Omnipod 5, we offer:
- Omnipod 5 10-Day Free Trial†
- Let your patients try Omnipod 5 with a free Intro Kit (Controller and 10 Pods)
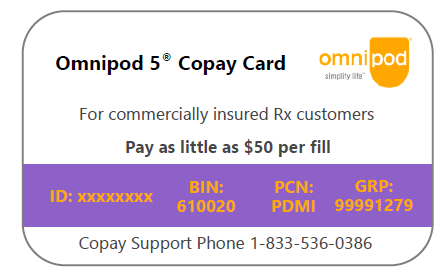
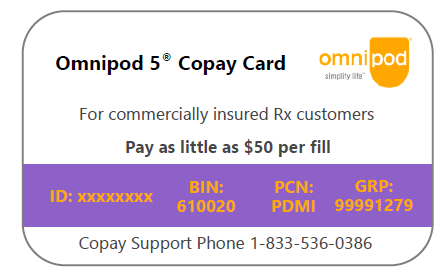
- Omnipod 5 Copay Card§
- For patients with hesitancy due to cost, the Copay card may buy down their monthly Copay to $50 with a max buy down of $100 (Copay card benefit can be applied monthly, for one year only)
Who is Eligible?
Your patients may be eligible for both the Omnipod 5 Free Trial** and the Omnipod 5 Copay Card, if:
- They have a commercial or private insurance (no government insurance) AND
- Their insurance plan covers Omnipod 5.
How to Get Patients Started with the Omnipod 5 Free Trial and Copay Card**
1. E-scribe both the Intro Kit and refill Pods to ASPN Pharmacies using your EHR.
2. Both of the following prescriptions need to be sent to ASPN Pharmacies to get your patient started on the Omnipod 5 AID system‡
| Omnipod 5 G6 Intro Kit (Gen 5) |
| Use as directed |
| Qty 1 |
| 0 refills |
| NDC #: 08508-3000-01 |
| Omnipod 5 G6 Pods (Gen 5) Refill 5-Pack |
| Use as directed |
| Qty 2 boxes (30 day supply) |
| 11 refills |
| NDC #: 08508-3000-21 |
‡ If your patient isn’t already on the Dexcom G6, the Dexcom G6 requires a separate prescription and is necessary to use Omnipod 5 in Automated Mode. When prescribing Free Trial to your patient not currently on Dexcom G6, they can get started with a Dexcom sample by visiting Dexcom.com/SampleOP5.
3. ASPN Pharmacies will verify eligibility for both the Free Trial and the Copay card for Pod refills. They will also communicate the Copay for Pod refills and help coordinate fulfillment at the patient’s preferred pharmacy.
For any questions, you can call ASPN pharmacies at: 1-866-347-0036
Financial Assistance Programs May be Available4
Have your patients visit https://www.omnipod.com/financial-assistance or call customer care at 1‑800‑591‑3455 to learn more.
1. Reflects coverage for Omnipod 5 G6 Intro Kit and Omnipod 5 G6 Pods. Source: Insulet Data on File As of June 1 2023.
2. Calculated based on a consumption of ten (10) Pods per month. Majority defined as at least 70% of patient co-pays $50 or less per month . Among All Paid Omnipod 5 G6 Pods Commercial and Medicare Claims from August 2022 through July 2023. Includes benefits and offerings available through Insulet, such as the copay card program. Actual co-pay amount depends on patient’s health plan and coverage, they may fluctuate and be higher or lower than the advertised amount on a monthly basis. Source: IQVIA OPC Library. Calculated based on a consumption of ten (10) Pods per month. Among All Paid Omnipod 5 G6 Pods Commercial and Medicare Claims from August 2022 through July 2023. Includes benefits and offerings available through Insulet, such as the copay card program. Actual co-pay amount depends on patient’s health plan and coverage, they may fluctuate and be higher or lower than the advertised amount on a monthly basis. Source: IQVIA OPC Library
3. Calculated based on the proportion of script fills within 24-hour look forward period out of all script fills within a 90-day look forward period among all new to brand claims for the Omnipod 5 G6 Intro Kit from October 2022 to March 2023. Excludes claim reversals. Source: IQVIA Payer Control Library
†Omnipod® 5 10-Day Free Trial
Terms and Conditions
1. Program Eligibility
Eligibility criteria: Subject to program limitations and terms and conditions, the Omnipod 5 10-day Free Trial Program (the “Program”) is open to patients who have a valid Omnipod 5 and Dexcom G6 prescription and who have commercial or private insurance, including plans available through state and federal healthcare exchanges. In order to be eligible, the patient’s eligible insurance plan must include coverage for Omnipod 5 Pods. The Program is open to new Pod Therapy patients coming from multiple daily injections or tubed pumps only who have not previously used Omnipod 5, Omnipod DASH®️ or Omnipod Insulin Management System.
This offer is not valid for participants whose Omnipod 5 or Dexcom G6 prescription is paid for in whole or in part by Medicare, Medicaid, or any other federal or state programs. It is not valid for cash-paying participants or where prohibited by law. A participant is considered cash-paying where the participant has no insurance coverage for Omnipod 5 or where the participant has commercial or private insurance but Insulet determines in its sole discretion the participant is effectively uninsured because such coverage does not provide a material level of financial assistance for the cost of an Omnipod 5 prescription. Participants on certain commercial insurance plans may not be eligible. This offer is only valid in the United States, Puerto Rico, and the U.S. territories. Participants receiving their products through the Durable Medical Equipment or Pharmacy Durable Medical Equipment channel are not eligible to participate in the copay card program. Please contact Insulet Customer Support at 1-800-591-3455 for details.
2. Program Details
With this program, Participants may be eligible to receive a limited supply of Omnipod 5 products at no cost for them. Eligible participants have two (2) options, based on the following:
• A participant shall sign the Try Omnipod 5 Free Trial Acknowledgement through the appropriate platform provided by Insulet.
• Once Insulet has received the request, the request shall be escalated to Insulet’s pharmacy partner, where a request for a prescription shall be sent to the participant’s healthcare professional. If a valid prescription is received, both for the Omnipod 5 Intro Kit and the Omnipod 5 Pods, the participant’s benefits will be checked by Insulet or its partners.
• IF the benefits check results in a monthly copay equal to or below two hundred dollars ($200), then Insulet shall issue a one-time only copay card to the participant, for a value equal to the out-of-pocket expenses the participant would have to pay for an Omnipod 5 Intro Kit, in accordance with Section 3, below.
• IF the benefits check result in a copay greater than two hundred dollars ($200), Insulet, or its authorized partners, shall arrange for the shipment of one (1) Omnipod 5 Intro Kit, in accordance with Section 4, below.
• For the purpose of clarity, the term “copay” shall encompass any out-of-pocket expense for one (1) month’s supply of Pods, including any deductible, copays and other out-of-pocket expenses that the participant would have to disburse to procure said supply of Pods.
• Any copay assistance may not apply to a participant’s health plan’s deductible if prohibited by state law or by a health plan.
• In order to use the Omnipod 5 System in Automated Mode, the User must also procure a Dexcom G6 Continuous Glucose Monitor System. For more information about how to obtain a 10-day supply of Dexcom G6, please contact Dexcom or click on the following link: http://www.dexcom.com/SampleOP5.
Insulet reserves the right to change, amend or rescind this Program, in whole or in part, at any time.
3. Copay Card
Should participant be deemed eligible to receive an Omnipod 5 Copay Card, participant shall receive electronically one (1) Omnipod 5 Copay Card, valid for a single use, in the amount required for the participant to procure one (1) Omnipod 5 Intro Kit, which shall include:
• One (1) Omnipod 5 Controller
• Ten (10) Omnipod 5 Pods
• One (1) Omnipod 5 Guide
• One (1) Controller charging cable
4. Product Dispense
Should participant be deemed eligible to receive a one-time dispense of Omnipod 5 Pods at no cost to them, Insulet, or its authorized partner, shall dispense one (1) Omnipod 5 Intro Kit, which shall include:
• One (1) Omnipod 5 Controller
• Ten (10) Omnipod 5 Pods
• One (1) Omnipod 5 Guide
• One (1) Controller charging cable
The Omnipod 5 Intro Kit shall be delivered to the shipping address indicated by participant in their Acknowledgment Form. Any estimate date of delivery is given solely for participant’s information and does not constitute a warranty that the Intro Kit will be delivered on said date. Participant is responsible to provide an accurate delivery address, to receive shipment of the Intro Kit and to verify the content of the Intro Kit.
§ Omnipod 5 Copay Card Program
Terms and Conditions
1. Program Eligibility
Eligibility criteria: Subject to program limitations and terms and conditions, the Omnipod 5 Copay card program (the “Program”) is open to patients who have a valid Omnipod 5 prescription and who have commercial or private insurance, including plans available through state and federal healthcare exchanges. This offer is not valid for participants whose Omnipod 5 prescription is paid for in whole or in part by Medicare, Medicaid, or any other federal or state program. It is not valid for cash-paying participants or where prohibited by law. A participant is considered cash-paying where the participant has no insurance coverage for Omnipod 5 or where the participant has commercial or private insurance but Insulet determines in its sole discretion the participant is effectively uninsured because such coverage does not provide a material level of financial assistance for the cost of an Omnipod 5 prescription. This offer is only valid in the United States, Puerto Rico, and the U.S. territories. Participants receiving their products through the Durable Medical Equipment or Pharmacy Durable Medical Equipment channel are not eligible to participate in the copay card program. Participants on certain commercial insurance plans may not be eligible. Please contact Insulet Customer Support at 1-800-591-3455 for details.
2. Program Details
With the Program, a commercially insured participant who meets eligibility criteria may pay as little as a $50 copay per month for their Omnipod 5 monthly out-of-pocket costs. For all eligible participants, the Program offers:
• A program benefit that covers the participant’s eligible out-of-pocket prescription costs for Omnipod 5 Pods (copay, deductible, or co-insurance) on behalf of the participant, up to a Maximum Monthly Benefit and/or a Maximum Annual Benefit.
• A program benefit that covers the participant’s eligible out-of-pocket prescription costs for Omnipod 5 Pods (copay, deductible, or co-insurance) on behalf of the participant, up to a Maximum Monthly Benefit and/or a Maximum Annual Benefit.
• The copay card covers a thirty (30) days’ fill of Pods.
• The Program offers to participants a Maximum Monthly Benefit of up to $100. The actual monthly benefit depends on the participant’s out-of-pocket costs, for a copay target of $50. The Participant’s monthly benefit are unilaterally determined by Insulet in its sole discretion (not to exceed the Maximum Monthly Benefit). The monthly benefit may be less than the Maximum Monthly Benefit based on the participant’s insurance coverage and the copay target of $50. For the purpose of clarity and as an example, a participant with a copay of $75 shall receive a monthly benefit of $25, to bring the copay to $50. Similarly, a participant with a copay of $200 shall receive a monthly benefit of $100, to bring the copay to $100.
• The Maximum Annual Benefit may be up to $1200. The actual Maximum Annual Benefit shall vary depending on each participant’s actual monthly benefits throughout the year.
• The participant shall not receive any benefit if at any point their monthly copay is equal to or lower than $50.
• The participant shall not receive a monthly benefit of more than $100, even if the target copay of $50 is not reached, when the participant’s monthly copay is greater than $150.
• Participants are solely responsible for updating Insulet with changes to their prescription or health insurance, including but not limited to, initiation of insurance provided by the government, in addition to any change in coverage terms or other offers such as accumulator adjustment benefit design or copay maximization programs. Participants shall further inform Insulet of any change or lapse in coverage for Omnipod 5.
• Participants are responsible to provide Insulet with accurate information on their copay.
• Participants may use the card every time they fill their Omnipod 5 prescription.
• The copay card covers only Omnipod 5 Pods, and does not apply to any out-of-pocket expenses from third parties suppliers, including, but not limited to, continuous glucose monitors or other diabetes-related supplies. Insulet reserves the right to change, amend or rescind this Program, in whole or in part, at any time.
3. Limitations
The Program may not be combined with any other offer, rebate or coupon. If at any point a participant begins receiving coverage under any state or government program, the participant will no longer be able to use this card and they must contact Insulet Customer care at 1-800-591-3455 to stop their participation. Participating in this Program means that you are ensuring you comply with any required disclosure regarding your participation in the Program. Other restrictions may apply. Health plans, specialty pharmacies and Pharmacy Benefits Managers not specifically authorized by Insulet are prohibited from enrolling participants in the Program. The copay card shall last for a maximum of twelve (12) months per participant. This Program is not health insurance. Insulet reserves the right to rescind, revoke or amend this offer, as well as any eligibility criterion without further notice.
4 Omnipod® Copay Card
Financial Assistance Program Terms
1. Program Eligibility
Eligibility criteria: Subject to program limitations and terms and conditions, the Omnipod® Financial Assistance Program (the “Program”) is open to patients who have a valid Omnipod DASH® or Omnipod® 5 prescription who demonstrate a financial need for assistance based on criteria established by Insulet, and who fill their prescription through the Pharmacy channel.
This offer is not valid for participants whose prescription is paid for in whole or in part by Medicare, Medicaid, or any other federal or state program. This offer is only valid in the United States, Puerto Rico, and the U.S. territories. Participants receiving their products through the Durable Medical Equipment or Pharmacy Durable Medical Equipment channel are not eligible to participate in the copay card program. Participants on certain commercial insurance plans may not be eligible. Please contact Insulet Customer Support at 1-800-591-3455 for details.
2. Program Details
With the Program, an approved participant who meets eligibility criteria may receive a copay card to reduce their monthly out-of-pocket expenses when filling their Omnipod® prescription. The program is described as follows:
• A program benefit that covers the participant’s eligible out-of-pocket prescription costs for Omnipod DASH® and Omnipod® 5 Pods (copay, deductible, or co-insurance) on behalf of the participant, in accordance with criteria determined by Insulet.
• In order to participate in the Program, a person shall complete Insulet’s Financial Assistance Program Application Form, as provided by Insulet and as may be updated from time to time.
• The form shall be filled out with true and correct information by the applicant and provided to Insulet.
• In addition, the applicant shall provide evidence of income, as directed by Insulet.
• Insulet shall evaluate the application in accordance with its policies and make a determination as to the eligibility of the applicant.
• If the application is accepted by Insulet, Insulet shall communicate to the participant the level of assistance that they will receive as part of the Program.
• The assistance shall be provided through a copay card delivered electronically by Insulet to Participant.
• The copay card shall be valid for one (1) year and covers a thirty (30) days’ fill of Pods, every month.
• Participants are solely responsible for updating Insulet with changes to their prescription, financial situation or health insurance, including but not limited to, initiation of insurance provided by the government, in addition to any change in coverage terms or other offers such as accumulator adjustment benefit design or copay maximization programs. Participants shall further inform Insulet of any change or lapse in coverage for their Omnipod ® prescription.
• Participants are responsible to provide Insulet with accurate information on their copay.
Insulet reserves the right to change, amend or rescind this Program, in whole or in part, at any time.
3. Limitations
The Program may not be combined with any other offer, rebate or coupon. If at any point a participant begins receiving coverage under any state or government program, the participant will no longer be able to use this card and they must contact Insulet Customer care at 1-800-591-3455 to stop their participation. Participant shall also update Insulet if their financial situation changes in a way that would make them non-eligible to participate in the Financial Assistance Program. Participating in this Program means that you are ensuring you comply with any required disclosure regarding your participation in the Program. Other restrictions may apply. Health plans, specialty pharmacies and Pharmacy Benefits Managers not specifically authorized by Insulet are prohibited from enrolling participants in the Program. The copay card shall last for a maximum of twelve (12) months per participant.
This Program is not health insurance. Insulet reserves the right to rescind, revoke or amend this offer, as well as any eligibility criterion without further notice.
INS-OHS-05-2023-00055 V1.0